Dietary interventions as now conducted are incapable of rendering valid causal conclusions about specific substances, compounds, or chemicals. This is because the near-infinite variations in foods produce unknown and unknowable co-contamination errors that are further confounded by preparation inconsistencies.
This ad-free article is made possible by the financial support of the
Center for Research on Environmental Chemicals in Humans: a 501(c)(3) non-profit.
Please consider making a tax-deductible donation for continued biomedical research.
This can be illustrated by comparing two recent dietary intervention studies — one studying Plastic-Derived Chemicals (Reus, Perdue) and the second of Ultra-Processed Foods (NIH/Hall). While the two studies were quite different in scope, size, and duration, they arrived at very similar results in the behavior of the high-sensitivity C-Reactive Protein (hsCRP) test as a clinical measure of intervention inflammation changes.
The NIH/Hall study, “Ultra-Processed Diets Cause Excess Calorie Intake and Weight Gain,” was a 28-day trial published in the May 16, 2019 issue of Cell Metabolism and represented the most thoroughly documented dietary intervention published so far. In addition to documenting the association between Ultra-Processed Foods (UPFs) and weight gain from over-eating, the study was conducted in a dormitory setting to compensate for non-food environmental exposures, test subject compliance and differences in exercise, and metabolism. In addition, the study conducted an expensive battery of clinical tests (op. cit. Table 3) including hsCRP, insulin, and the appetite peptides leptin, ghrelin, and adiponectin.
The Reus, Perdue six-day trial was far more limited in scope and sought primarily to determine whether hsCRP levels could be affected by Bisphenol A and other commonly associated Plastic-Derived Chemicals (PDCs). Extensive efforts conducted by investigators over a period of more than three years to determine which foods, sources, packaging, and preparation methods were least — and most — contaminated by PDCs. That work included efforts to:
- develop a set of protocols and best practices to avoid PDC contamination in sourcing and preparation,
- determine how the food chain gets contaminated with PFCs, and
- ascertain how food processing adds PDC contamination.
Among the data and methods developed by the Reus, Perdue investigators in that pre-trial effort was the determination that fast, convenient, ready-to eat, and pre-prepared — Ultra-Processed — foods were the most contaminated by PDCs. For that reason, UPFs were often chosen for the “contamination” leg of the study. Intervention leg meals were “reverse engineered” to match the composition of the UPFs in order to make the”before and after” legs as identical as possible save for PDC contamination.
Within days of the publication of the NIH/Hall study, Reus, Perdue investigators initially considered replicating the “before and after” selections of that extensive study and requested recipes. No response was ever made. A thorough examination of supplemental material from NIH/Hall failed to find recipes or any food sourcing and preparation details.
In the interim, a closer examination by the Reus, Perdue investigators revealed that the NIH/Hall intervention meals included foods that the Reus, Perdue investigators had previously determined had been processed more than minimally and likely contained higher PDC levels than desired.
Similar results and an anomaly indicate unavoidable mutual co-contaminants that confounded both dietary interventions and negated causal conclusions
Levels of hsCRP decreased 21.4% from baseline to end of the minimally contaminated leg: 1.1 mg/L from 1.4 mg/L. In addition, our study results demonstrated a final reduction in hsCRP that was approximately half of that reposted by a major NIH-funded dietary intervention by Hall, et. al. published in 2019 approximately four months prior to our trial.
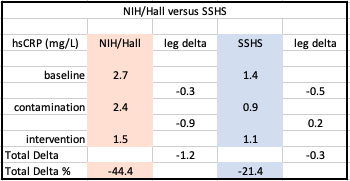
NIH/Hall data from: “Ultra-Processed Diets Cause Excess Calorie Intake and Weight Gain: An Inpatient Randomized Controlled Trial of Ad Libitum Food Intake”
The lower overall decrease in hsCRP in the Reus, Perdue study was reasonably attributable to:
- The shorter duration of our trial (six days rather than 28), and
- The Northern California wildfires of November/December 2019, whose smoke pollution dramatically increased PM2.5 particulate which is a notorious promoter of inflammation.
Further discussion is available in the Reus, Perdue study.
Investigating An Unexpected Anomaly of the Intervention Legs
Despite expectations that inflammation would increase with foods projected to contain higher levels of BPA, hsCRP actually declined at the end of the “typical/contaminated” diet leg. Significantly, NIH/Hall independently exhibited this same anomaly.
Efforts to explain this anomaly led investigators to consider possible causes.
NIH/Hall’s primary outcome focused on obesity and investigated weight gain from the ad libitum consumption of UPFs versus less processed foods. The results confirmed weight gain from the contaminated UPF leg of the study.
In looking for a possible cause of the anomaly of how BPA, hsCRP counterintuitively declined at the end of the “typical/contaminated” diet, Reus, Perdue study investigators had long recognized that Bisphenol A has been widely accepted as an “obesegen<Google Scholar cite>” and associated with obesity, diabetes, insulin dependence, as well as cancer and cardiovascular disease.
Further, chronic inflammation is associated with all of those syndromes and non-communicable diseases. That was a primary reason Reus, Perdue study investigators had chosen hsCRP as a marker for PDC concentrations.
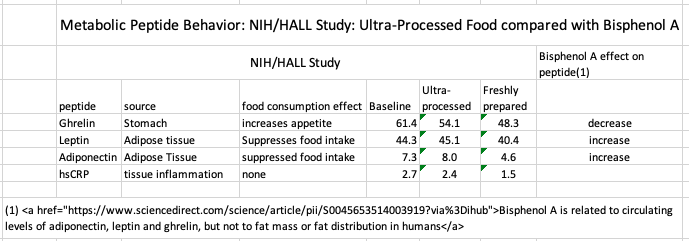
The NIH/Hall study included the “appetite peptides” ghrelin, leptin, and adiponectin which we previously knew were associated with eating behavior. Because of that, the Reus, Perdue investigators searched the literature for relevant BPA clinical markers of health outcome associations.
Data revealed that Bisphenol A affected ghrelin, leptin, and adiponectin affected in the ways as the NIH/Hall study recorded for Ultra-Processed Foods.
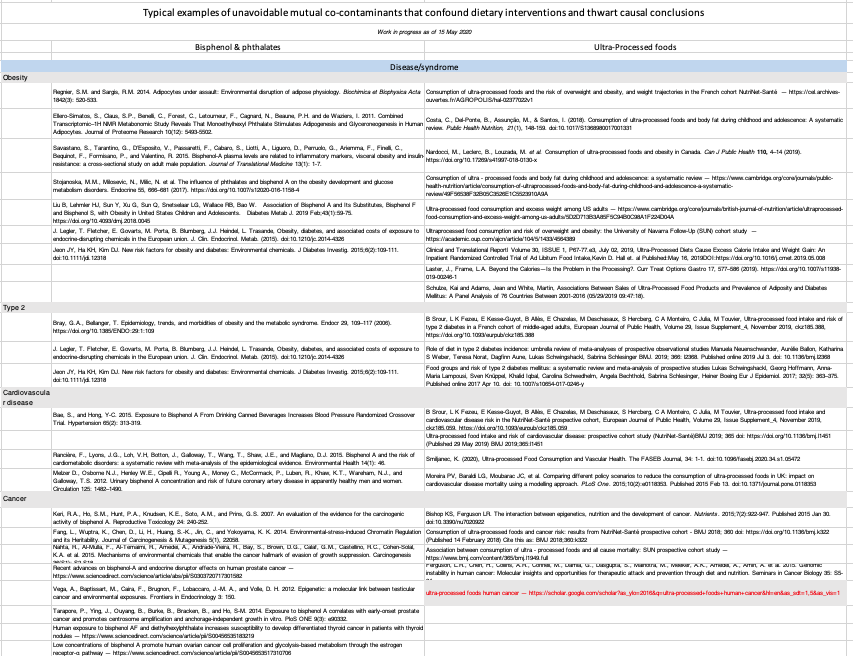
A further search for disease/syndromes and clinical indicator similarities between Plastic-Derived Chemicals and Ultra-Processed Foods (table below) further confirms that both show nearly identical activity. From this, the only conclusion that can be reached is that neither trial can delineate a specific causal action of PDC’s or UPFs because both are present in study foods, exert almost identical effects and are, therefore, mutually confounding factors.
The path to a revised protocol: Confounding factors lead to greater complexity and expense
This study’s investigators, from the beginning, recognized that basic nutritional levels — protein, fat, and sugar/carbohydrates would need to be the same at each level of the study. While unnecessary in previous dietary intervention studies that measured only BPA levels, the present study also measures health effects which can be affected by nutritional composition.
The widespread variance in BPA concentrations in source foods led to the realization that the reproducibility of this study would require testing of all source food for BPA concentrations. Otherwise, any record of increase or decrease in subject BPA concentrations would be invalid.
That recognition led to the conclusion that a reproducible investigation required the establishment of specific baseline food concentrations — leading to accurate dose levels of BPA consumed.
Investigators’ further research indicated that the American food chain is contaminated at every level by BPA and phthalates. The resulting food sourcing and testing demands increased the costs of the study far beyond the previous budget and would require extraordinary — and expensive — food production and processing methods to be implemented at the farm level and continuing in a highly controlled regime through processing, and preparation for table consumption.
This would require massive financial and personnel resources that make any such study impractical. to explore a less-expensive, causal and replicable method, please see: Significant changes necessary in order for dietary intervention studies to be causal and replicable